What is Giving Compass?
We connect donors to learning resources and ways to support community-led solutions. Learn more about us.
Serious psychiatric illness, also referred to as serious mental illness, includes major depressive disorder, schizophrenia, bipolar disorder, suicidality and other brain diseases that substantially interfere with one or more major life activities (NIMH, 2021). In young adults, the prevalence of serious mental illness affects 9% of youth between 18-25 years of age (NIMH, 2021).
Even though there are no cures for serious psychiatric illness, we know that it can often be effectively managed with interventions such as medication and therapy. However, despite the potential for recovery, it has been reported that less than one-third of youth with mental health difficulties seek or access healthcare services (Merikangas et al., 2011).
The COVID-19 pandemic and the recent widespread social unrest has affected society’s collective mental health, giving proof to how genetic, environmental, and social factors influence the development and progression of serious mental illness (NASEM, 2020). We also know that no single organization can independently address these complex and interacting factors, but coordinated and collaborative activities that focus on early detection and intervention will work best.
These influencers are the basis to why One Mind’s Accelerating Serious Psychiatric Illness Recovery (ASPIRe) initiative focuses on youth mental health and four components that are essential to changing the trajectory on a nationwide scale:
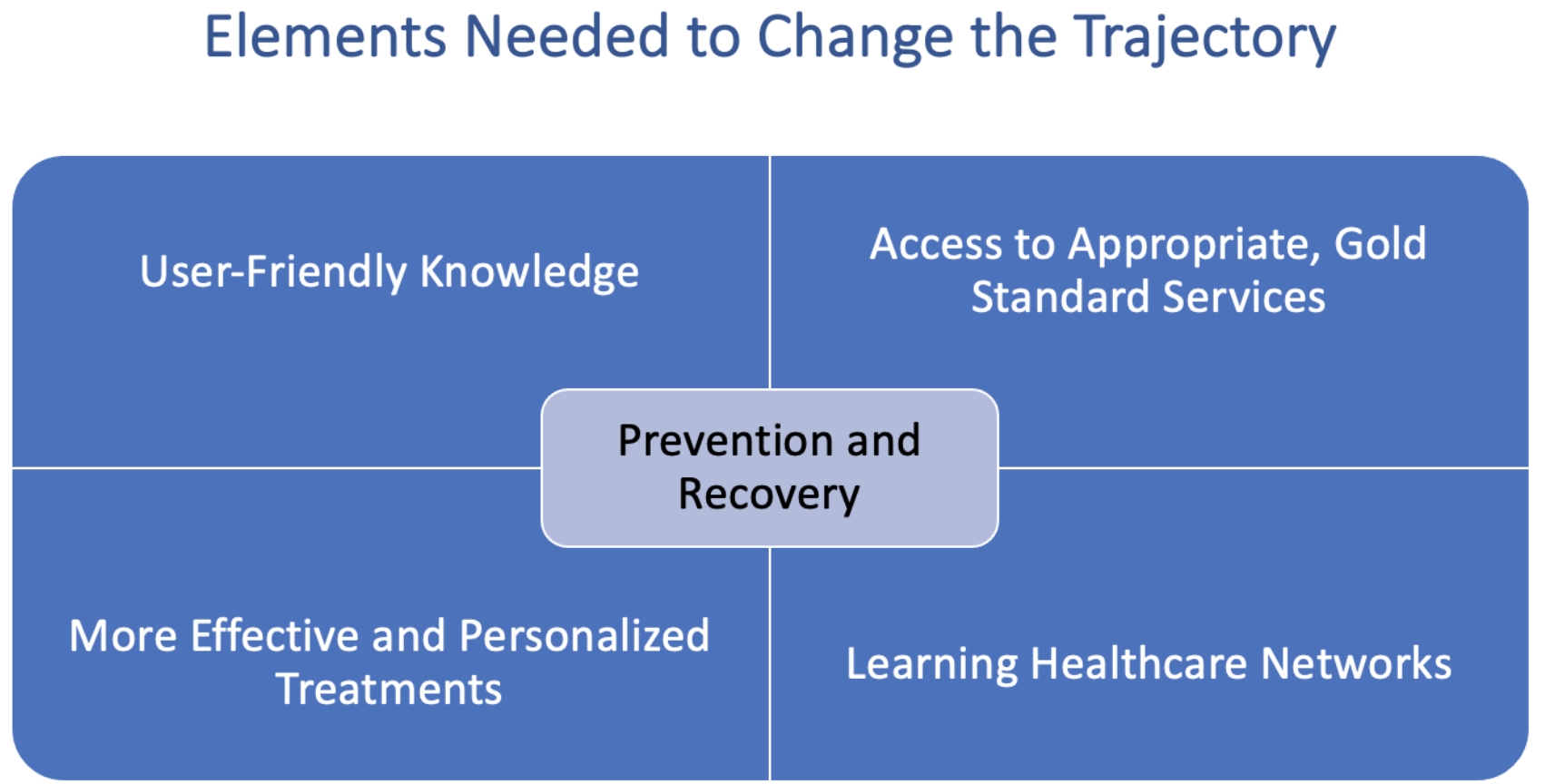
1. User-friendly Knowledge:
One reason that many individuals and families do not seek help or follow through with care is the stigma surrounding psychosis and their despair about the potential for recovery (Kaushik et al., 2016). Access to understandable, well-vetted research data, peer perspectives and advice from mental health experts can normalize mental health and strengthen the hope and knowledge needed to empower patients to make informed decisions.
One Mind All Media works to enable large-scale dissemination of this knowledge using a variety of media platforms. Current efforts include Brain Waves, a weekly webcast series that interviews scientists and persons with lived experience, our annual Scientific Symposium, and major partnerships such as the nationally focused Well Beings public media campaign and McCarter Theatre Center's The Manic Monologues.
2. Access to Appropriate Gold Standard Services:
Early intervention that identifies youth at risk for mental illness is a key driver for the prevention and recovery from serious psychiatric illness.
Although there are several screening tools available for evaluating youth mental health, concerns have been voiced about their effectiveness. To address these concerns, One Mind established a think tank on youth mental health to guide the development of an effective screening tool that can be scaled up nationwide. In addition, One Mind’s Strong365 is developing a platform for digital outreach that connects individuals seeking information about psychosis online with referrals to high quality treatment centers and other resources.
Early intervention also requires access to effective and affordable mental health care. We estimate that the current capacity for coordinated specialty care (CSC), which is considered the “gold standard” for psychosis, is less than 10% of what is needed. Another barrier is the affordability, influenced by the lack of billing codes for insurance providers.
To address these barriers, One Mind helped establish the Elizabeth Morgan Brown Center that is serving as a model for other coordinated specialty care programs we launch in California and beyond. To address the issue of affordability, we are working with providers, payers, and policy groups to develop fair and reasonable reimbursement policies.
3. More Effective and Personalized Treatments
The limitations in current diagnostics and treatments for youth with serious mental illness is arguably the greatest reason for underutilization of services. Diagnosis is currently reliant on symptomatology, with a large overlap across mental health and neurological disorders, that prolongs or even prevents accurate diagnosis. Diagnostic tools that are based on biological indicators (biomarkers) will shorten the time and increase the accuracy and enable the development of more targeted therapies with fewer unwanted side effects.
Developing such biomarkers is one of the major objectives of the Accelerating Medicines Partnership - Schizophrenia (AMP-SCZ), which is coordinated by the Foundation for NIH and includes One Mind and other industry and nonprofit organizations. Scalability is likely because of the partnerships with research organizations, regulatory agencies, advocacy groups, and industry.
4. Learning Health Care Networks
Much remains unknown about which aspects of coordinated specialty care are most effective and for whom. To help confirm the effectiveness of the CSC model, in collaboration with the State of California Mental Health Research and Oversight Commission, One Mind is supporting EPI-CAL, a learning health care network for community-based providers among 10 counties in California that has also been selected to join a larger, NIH-funded network called EPINET that will provide opportunities for collaboration nationally. Strategies for learning healthcare networks that emerge from EPI-CAL can be applied to other serious psychiatric illnesses in the future.
Ways to Get Involved
- Invest in mental health by supporting the One Mind ASPIRe initiative.
- Educate yourself about mental health via One Mind’s Brain Health Library and our One Mind Brain Waves webcast series.
Connect with The Kennedy Forum to ensure that policymakers have the tools they need to craft better policy and to improve the affordability of care.
____
Original contribution by Garett Slettebak, Director of Marketing & Communications at One Mind.