Giving Compass' Take:
- Emily M. Godfrey and Adelaide H. McClintock explain that in the post-Roe landscape, primary care has essential roles to play in supporting reproductive healthcare.
- How can you work to increase access to quality primary care and reproductive, particularly in places where abortion access is restricted?
- Find state-by-state abortion access information.
What is Giving Compass?
We connect donors to learning resources and ways to support community-led solutions. Learn more about us.
Just over a month after the Supreme Court struck down 50 years of federal protection of abortion rights in the U.S., at least 43 abortion clinics in 11 states have stopped offering abortion services. In states where abortion remains legal, abortion clinics are experiencing excessive wait times due to the influx of out-of-state patients.
Wait times are only expected to grow as more states restrict abortion with regulations such as gestational age limits, waiting periods and requirements for in-person visits, unnecessary clinical tests and required parental consent for minors. Abortion bans and restrictions are associated with higher rates of complications and are harmful to the health of women because they delay necessary care.
Although primary care doctors and clinicians are not typically associated with the abortion debate, they are a critical, untapped resource to help offset the abortion care crisis. Primary care is a key access point for patients, especially for adolescent, low-income and rural women.
And because almost all Americans value their relationship with their primary care provider, primary care has a responsibility to ensure patients maintain personal bodily autonomy, including deciding when and how many children to have.
In the post-Roe era, primary care providers can help their patients prevent unintended pregnancy and avoid delays in abortion care by providing comprehensive contraceptive and family planning services, knowing how to counsel and refer individuals seeking pregnancy termination and providing post-abortion care. Due to various state restrictions, providers should familiarize themselves with their specific state regulations to determine what is permissible in their current practice environment.
We are practicing primary care physicians who include comprehensive family planning as part of our practices. We have written extensively about the feasibility of including full-spectrum birth control and first-trimester abortion services in primary care.
Primary care providers make up 30% of the entire U.S. clinician workforce. They include family physicians, general internists, pediatricians and advanced practice clinicians such as nurse practitioners, midwives and physician assistants, who are often the only source of care in underserved and rural areas.
Primary care’s role in preventing abortion
One of the top reasons why patients go to their primary care provider is for birth control. Primary care clinics that provide all-inclusive birth control services reduce unintended pregnancy rates in their communities, which can help alleviate the demand for abortion services.
Primary care providers can talk with their patients about becoming pregnant now or in the future, using clinical tools that help patients decide which birth control method to use.
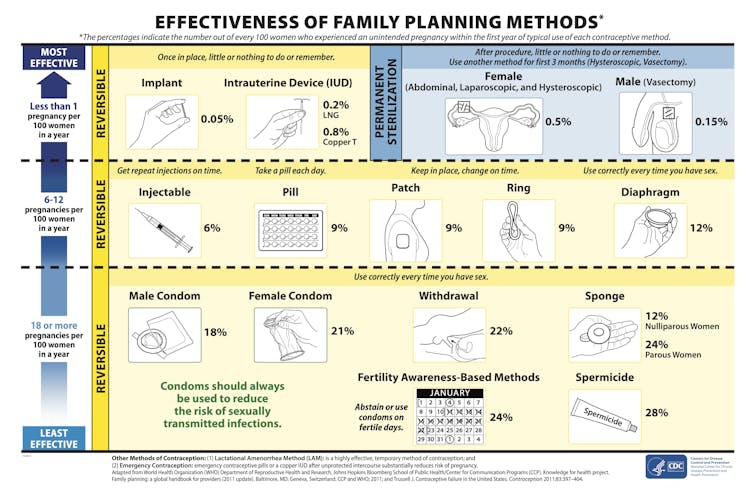
Centers for Disease Control and Prevention
Nationally based birth control clinical guidelines empower clinicians to prescribe even the most effective birth control methods, such as an implant or intrauterine device – IUD – to patients with serious and chronic medical conditions. Primary care can also help patients with emergency contraception, either in the form of a pill or IUD, within five days after unprotected sex.
Emergency contraceptive pills are considered safe and effective. They are high-dose birth control pills that work by interfering with the process of ovulation, and thus will not affect a pregnancy if already pregnant. Emergency contraception is a last chance to prevent unplanned pregnancy.
Abortion pill prescription falls within primary care
Abortion with medications can be safely and effectively used up to the 11th week of pregnancy, with low rates of complications. Of the approximately 1 million legal abortions provided each year in the U.S., 90% occur in the first trimester, or through the 12th week of pregnancy. Thus, it’s no surprise that more than half of abortions are now managed with medicines that can be prescribed by a primary care provider.
The National Academies of Sciences, Engineering and Medicine have issued evidence-based guidelines reiterating that trained, licensed primary care clinicians can safely and effectively provide medication abortion. Patients who have received abortions from primary care providers report that they are satisfied with the experience. Studies show that patients prefer abortion services in primary care because of the privacy, convenience and continuity of care.
How abortion care can be integrated into telehealth
Despite the fact that first-trimester abortion care fits well within primary care medical services, it has not been widely offered in this setting. This is due to roadblocks, including lack of provider training, federal and state legislation, institutional barriers and administrative resistance.
However, there are now new, more simplified medication abortion protocols that allow primary care to safely offer abortion care remotely with a history screening tool that doesn’t require unnecessary clinical laboratory and ultrasound testing. Primary care’s expansion of telehealth abortion services has the potential to significantly reduce delays in care. This could help reduce abortions at more advanced gestational ages and the complications that come with them. Our study from 2021 conducted among primary care physicians providing telemedicine abortion found that more than 85% of patients were less than seven weeks pregnant when they sought care.
Post-abortion ‘primary’ care
In states with restricted abortion access, it is inevitable that patients will seek abortions on their own. Given the current legal landscape, clinicians are often confused about how to treat patients with pregnancy complications, including miscarriage. The World Health Organization stresses that even in settings where abortion may be outlawed, it is incumbent for clinicians to provide compassionate, nonjudgmental post-abortion care.
Post-abortion care includes managing residual side effects or complications of abortion, as well as the provision of comprehensive birth control services without discrimination or coercion. Complications from abortion or miscarriage are rare. However, complications like retained pregnancy tissue in the uterus, bleeding or infection can occur, most of which can be managed by primary care providers in the clinical setting.
Primary care providers who don’t offer abortion care can still counsel patients about where to seek reliable, high-quality abortion services. The U.S. Department of Health and Human Services provides information about Americans’ rights to reproductive health care.
The short-term implications of the Supreme Court decision remain uncertain as state legislators weigh public opinion among their constituents.
What remains certain in the post-Roe era, however, is that primary care continues to be among the most reliable resources in the U.S. for accurate information and safe reproductive health care services.
Emily M. Godfrey, Associate Professor of Family Medicine and Obstetrics & Gynecology, School of Medicine, University of Washington and Adelaide H. McClintock, Professor of Internal Medicine, University of Washington
This article is republished from The Conversation under a Creative Commons license. Read the original article. The Conversation is a nonprofit news source dedicated to spreading ideas and expertise from academia into the public discourse.